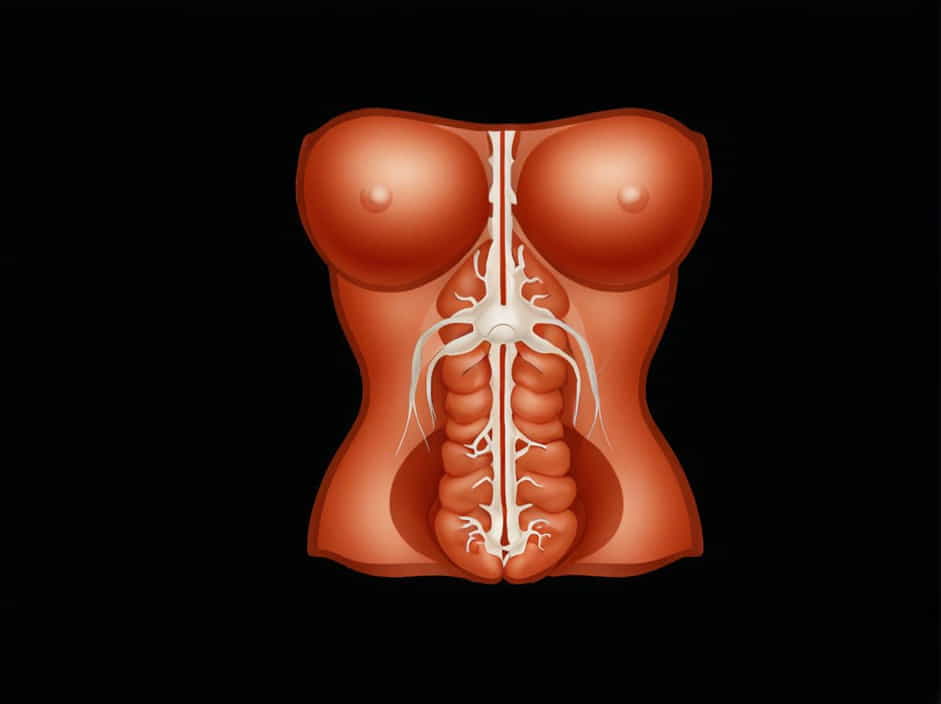
The abdominal viscera, including the stomach, intestines, liver, pancreas, and kidneys, rely on a complex network of nerves to regulate their functions. These nerves control digestion, secretion, blood flow, and pain sensation. The autonomic nervous system (ANS) plays a key role in this process, dividing into the sympathetic and parasympathetic nervous systems.
Understanding the nerve supply of the abdominal viscera is crucial for diagnosing and managing gastrointestinal disorders, pain syndromes, and autonomic dysfunctions.
Autonomic Nervous System and Abdominal Viscera
The autonomic nervous system (ANS) is responsible for the involuntary control of visceral organs. It is divided into:
- Sympathetic Nervous System (SNS): Activates the “fight or flight” response, reducing digestion and increasing blood flow to muscles.
- Parasympathetic Nervous System (PNS): Promotes the “rest and digest” state, enhancing digestion and organ function.
Both systems work together to maintain homeostasis in the abdominal organs.
Sympathetic Nerve Supply of Abdominal Viscera
The sympathetic nervous system (SNS) originates from the thoracolumbar region (T5-L2) of the spinal cord. It primarily controls vasoconstriction, inhibition of digestion, and stimulation of glucose release.
1. Thoracic Splanchnic Nerves
These nerves arise from the sympathetic trunk and supply various abdominal organs:
- Greater splanchnic nerve (T5-T9): Synapses in the celiac ganglion, supplying the stomach, liver, pancreas, and intestines.
- Lesser splanchnic nerve (T10-T11): Synapses in the superior mesenteric ganglion, innervating the midgut, including the small intestine and ascending colon.
- Least splanchnic nerve (T12): Synapses in the aorticorenal ganglion, supplying the kidneys and adrenal glands.
2. Lumbar Splanchnic Nerves (L1-L2)
These nerves synapse in the inferior mesenteric ganglion, controlling the hindgut (descending colon, rectum, and bladder).
3. Effects of Sympathetic Stimulation
- Decreased digestive secretions
- Reduced intestinal motility
- Constriction of blood vessels to abdominal organs
- Increased glucose release from the liver
Parasympathetic Nerve Supply of Abdominal Viscera
The parasympathetic nervous system (PNS) originates from the craniosacral regions (cranial nerves and sacral spinal cord). It stimulates digestion, secretion, and absorption of nutrients.
1. Vagus Nerve (Cranial Nerve X)
The vagus nerve provides parasympathetic innervation to most of the abdominal organs up to the midgut (small intestine and proximal colon).
Functions of the Vagus Nerve:
- Stimulates digestive enzyme secretion
- Increases peristalsis (gut motility)
- Enhances bile production for fat digestion
- Regulates heart rate via visceral reflexes
2. Pelvic Splanchnic Nerves (S2-S4)
These nerves innervate the hindgut (distal colon, rectum, and bladder), promoting:
- Relaxation of the anal sphincter
- Increased mucus secretion in the intestines
- Stimulation of peristalsis
Enteric Nervous System: The “Second Brain” of the Gut
The enteric nervous system (ENS) is an independent neural network within the gut wall, controlling digestion without direct brain input. It consists of:
- Myenteric plexus (Auerbach’s plexus): Regulates gut motility.
- Submucosal plexus (Meissner’s plexus): Controls secretions and blood flow.
The ENS communicates with the autonomic nervous system but can function independently, coordinating smooth muscle contractions and enzyme release.
Clinical Relevance of Abdominal Nerve Supply
1. Visceral Pain and Referred Pain
Abdominal pain is often poorly localized due to the diffuse nerve supply. Common referred pain patterns include:
- Stomach pain → Epigastric region (T5-T9)
- Gallbladder pain → Right upper quadrant and shoulder (T7-T9)
- Appendix pain → Initially periumbilical (T10), later localized to the right lower quadrant
2. Autonomic Dysfunction and Gastrointestinal Disorders
Nerve dysfunction can lead to various conditions:
- Gastroparesis (delayed stomach emptying): Often linked to vagus nerve damage (e.g., diabetes, surgery).
- Irritable Bowel Syndrome (IBS): May involve dysregulation of the enteric nervous system.
- Hirschsprung’s Disease: Congenital absence of ENS ganglia, causing severe constipation.
3. Surgical Considerations
Surgeons must carefully avoid nerve damage during procedures such as:
- Vagotomy: Performed to reduce stomach acid production in ulcers.
- Sympathectomy: Used for conditions like excessive sweating or chronic pain.
The nerve supply of the abdominal viscera is a complex interaction between the sympathetic, parasympathetic, and enteric nervous systems. These neural pathways regulate digestion, motility, and organ function.
A proper understanding of these nerves is essential for diagnosing gastrointestinal disorders, managing abdominal pain, and performing safe surgical procedures.