Understanding Aspergillus: Detection and Diagnosis Beyond X-rays
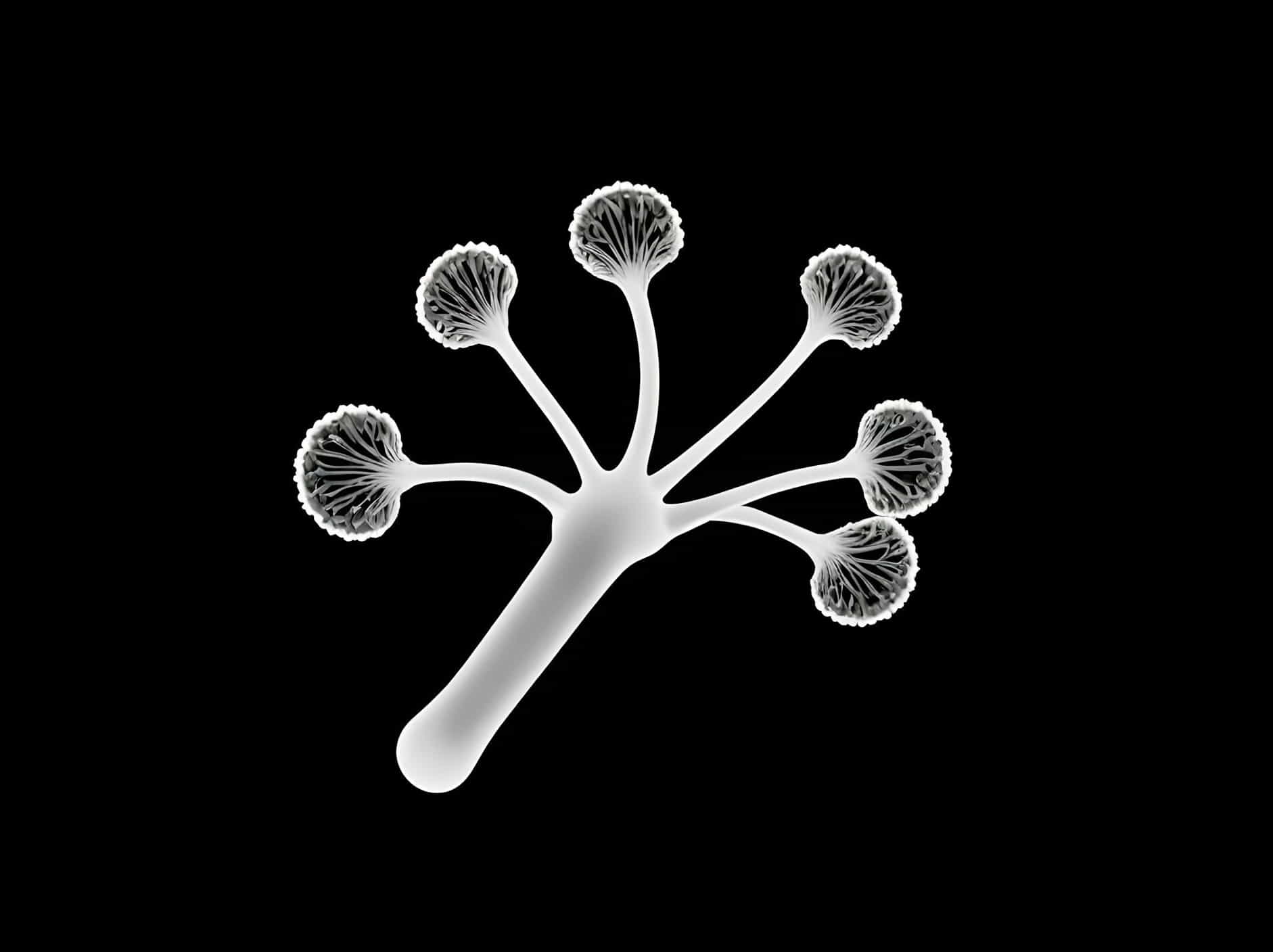
Aspergillus, a genus of mold found worldwide, encompasses several hundred species, but only a few are known to cause health issues in humans. Detection of Aspergillus in medical imaging, particularly X-rays, presents challenges due to its microscopic size and the nature of its impact on the human body. This article explores how Aspergillus is detected and diagnosed, emphasizing why X-rays alone may not be sufficient for accurate identification.
What is Aspergillus?
Aspergillus is a ubiquitous mold found in soil, decaying organic matter, and indoor environments such as homes and workplaces. While most people breathe in Aspergillus spores without harm, individuals with weakened immune systems or underlying respiratory conditions are at risk of developing infections.
Challenges in Detecting Aspergillus on X-rays
-
Microscopic Size: Aspergillus spores are extremely small, typically ranging from 2 to 8 micrometers in diameter. This size makes them difficult to detect using conventional X-ray imaging techniques, which are more suited to visualizing larger structures like bones and organs.
-
Radiological Features: Invasive forms of aspergillosis, such as invasive pulmonary aspergillosis (IPA), may present with nonspecific radiological findings on X-rays, such as nodular infiltrates or consolidations. These findings can resemble other lung infections or diseases, making it challenging to attribute them solely to Aspergillus without further diagnostic tests.
Diagnostic Approaches Beyond X-rays
-
Computed Tomography (CT) Scans: CT scans provide higher-resolution images than X-rays, allowing for better visualization of lung tissue and potential fungal infections like aspergillosis. CT scans can reveal characteristic patterns such as the “halo sign” or “crescent sign” associated with IPA, aiding in more accurate diagnosis.
-
Laboratory Tests: Direct examination and culture of respiratory samples, such as sputum or bronchoalveolar lavage (BAL) fluid, are crucial for identifying Aspergillus species and determining the appropriate antifungal treatment. These tests can confirm the presence of fungal elements and help differentiate between colonization and invasive disease.
-
Serological Tests: Blood tests for detecting specific antibodies or antigens associated with Aspergillus can complement imaging and culture-based methods, providing additional diagnostic information in suspected cases of fungal infections.
Clinical Presentation and Risk Factors
-
Immunocompromised Patients: Individuals with compromised immune systems, such as those undergoing chemotherapy or organ transplantation, are at increased risk of developing invasive aspergillosis. Prompt diagnosis and treatment are critical to improving outcomes in these vulnerable populations.
-
Chronic Lung Diseases: Patients with underlying conditions like cystic fibrosis or chronic obstructive pulmonary disease (COPD) may also be susceptible to Aspergillus infections, especially if their lung function is compromised.
Treatment and Management
Treatment of Aspergillus infections depends on the severity and type of infection:
-
Antifungal Therapy: Antifungal medications, such as voriconazole, are commonly used to treat invasive aspergillosis. Treatment duration and medication choice may vary based on the patient’s clinical condition and response to therapy.
-
Surgical Intervention: In some cases, surgical removal of infected lung tissue (lobectomy) may be necessary, especially if the infection does not respond to medical treatment or if there is a risk of life-threatening complications.
Prevention and Control Measures
-
Environmental Control: Minimizing exposure to Aspergillus spores in indoor environments through proper ventilation, moisture control, and regular cleaning of HVAC systems can reduce the risk of fungal infections.
-
Personal Protection: Individuals at higher risk of fungal infections, such as healthcare workers and construction workers, should use appropriate personal protective equipment (PPE) to prevent inhalation of fungal spores.
Conclusion: Beyond X-rays in Aspergillus Diagnosis
While X-rays can provide initial insights into pulmonary conditions, including those potentially caused by Aspergillus, their limitations in detecting fungal infections necessitate a multidisciplinary approach to diagnosis and management. Incorporating advanced imaging techniques, laboratory tests, and clinical evaluation is crucial for accurate identification of Aspergillus and timely initiation of appropriate treatment. By understanding the complexities of Aspergillus detection and diagnosis, healthcare professionals can optimize patient care and improve outcomes for individuals affected by fungal infections.